The retina is a thin sheet of nerve tissue in the back of the eye that contains photoreceptors. Light rays are focused onto the retina, then transmitted to the brain. The vitreous is a gel-like substance that fills the eye and is connected to the retina, optic nerve and many blood vessels. Problems with the retina and vitreous including retinal tear and detachment, macular degeneration, diabetic retinopathy, infection and trauma can lead to vision loss and blindness. Early detection and treatment are critical in correcting problems before vision is lost and preventing further deterioration from occurring.
Macular Degeneration
The macula is a part of the retina in the back of the eye that ensures that our central vision is clear and sharp. Age-related macular degeneration (AMD) occurs when the layer below the retina, called the retinal pigment epithelium (RPE) becomes diseased and stops functioning correctly. The RPE is important for keeping the overlying retina tissue healthy, and contains blood

vessels that supply the retina. Deprived of nutrients, the retinal tissues begin to weaken and die, causing vision loss. Patients may experience anything from a blurry, gray or distorted area to a blind spot in the center of vision.
AMD is the number-one cause of vision loss in patients 65 and older in the U.S. Macular degeneration doesn’t cause total blindness because it doesn’t affect the peripheral vision. Possible risk factors include genetics, age, diet, smoking and sunlight exposure. Regular eye exams are highly recommended to detect macular degeneration early and prevent permanent vision loss.
There are two kinds of AMD: wet (neovascular/exudative) and dry (non-neovascular). About 10-15% of people with AMD have the wet form. “Neovascular” means “new vessels.” Accordingly, wet AMD occurs when new blood vessels grow behind retina as the eye attempts to compensate for poor blood supply. These new vessels are very fragile, and often leak blood and fluid between the layers of the retina and under the retina. Not only does this leakage distort vision, but when the blood dries, scar tissue forms on the retina as well. This creates a dark spot in the patient’s vision. There are now medications that can be used to treat wet AMD, like Avastin, Eylea, and Lucentis. Intravitreal injections are performed in the office and deliver medication into the gel on the inside of the eye. They are used to treat a variety of ocular diseases, in particular those that cause macular edema (swelling that affects the central vision) or abnormal blood vessel growth in the eye. These diseases include macular degeneration, diabetic retinopathy, retinal vessel occlusions.
Dry AMD is much more common than wet AMD. Patients with this type of macular degeneration do not experience new vessel growth. Instead, symptoms include thinning of the retina, loss of retinal pigment and the formation of small, round particles under the retina called drusen. Vision loss with dry AMD is sometimes slower and often less severe than with wet AMD. Patients with dry AMD may be advised to take over-the-counter AREDS2 formulation vitmatins to reduce their risk of developing wet AMD.
Retinal Tear & Detachment
The vitreous is a clear substance that fills our eyes and gives them shape. When we are young, the vitreous has a thick, gelatinous consistency and is firmly attached to the retina. Over time, the vitreous thins and separates from the retina. Although this usually results in nothing more than a few harmless floaters, tension from the detached vitreous can sometimes tear the retina.
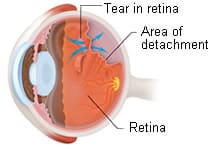
If liquid travels under the tear and collects behind the retina or between its nerve layers, the retinal tear can become a retinal detachment. Retinal detachment can cause significant, permanent vision loss and requires immediate medical attention.
There are three kinds of retinal detachment. The most common form, described above, occurs when fluid leaks into the retina; people who are nearsighted or who have had an injury or eye surgery are most susceptible. Less frequently, traction between the retina and vitreous or scar tissue pulls the retina loose, something that occurs most often in patients with diabetes. Third, disease-related swelling or bleeding under the retina can push it away from the eye wall.
Signs of retinal tear or detachment include flashes of light, a group or web of floaters, wavy or watery vision, a sense that there is a veil or curtain obstructing peripheral vision, or a sudden drop in vision quality. If you experience any of these symptoms, call your doctor immediately. Early treatment is essential to preserve your vision and is usually done through laser and cryoprobe procedures.
Retinal Vein Occlusion

Retinal vein occlusions are the second most common cause of blood vessel-related vision loss (the first is diabetic retinopathy). The condition occurs most often in men and women over the age of 50, particularly those in their 60s and 70s. Risk factors include high blood pressure, high cholesterol, diabetes, smoking, glaucoma, and, rarely, blood clotting and inflammatory conditions.
Treatment depends on the severity of the blockage and the location of the blocked vein. If the largest vein leaving the eye is affected, the condition is known as a central retinal vein occlusion, or CRVO; otherwise, it is called a branch retinal vein occlusion, or BRVO. BRVOs often occur with no pain or noticeable loss of vision. It is important to have routine eye exams to detect any developing problems early. You can keep tabs on your vision between appointments by closing one eye at a time.
Frequently Asked Questions: Retina
Question: I have floaters. Should I be concerned? Do I need an appointment?
Answer: Floaters are generally common, and in most cases are not a cause for immediate concern. If you see a floater or two in your vision every once in a while, you likely do not to see an eye doctor to evaluate. If you experience a sudden onset of a large number of floaters (and/or flashes of light or a curtain like shadow in your vision), it is indicative or a more serious issue. If this occurs with your vision, please give our office a call to schedule an appointment with one of our doctors, or Request an Appointment online.
Question: When do I need to see a Retina specialist instead of my Optometrist or General Ophthalmologist?
Answer: There are a few instances where a patient would need to see a Retina specialist instead of an Optometrist or General Ophthalmologist. If you have a retinal detachment or retinal tear, a Retina specialist is the type of Ophthalmologist you should be seeing for evaluation and possible surgery. Some patients also receive intravitreal injections for macular degeneration. These injections are typically done by Ophthalmologists who specialize in the Retina.